Friction on Your Skin
Friction produced from constant rubbing or pulling of your skin across surfaces can cause blisters. It should be avoided. Friction occurs when you drag any body part across a bed, toilet, or other surface during a transfer. Friction can also be caused by spasms. Your heels are a common site for this problem.
Dealing with Pressure Sores
Successful treatment of pressure sores requires removing the cause.
- Remove all pressure.
- Keep off the pressure sore.
- Keep the area around your sore clean and dry.
- May require bedrest with no sitting.
There are different ways to manage pressure sores after they have developed. Some may even require surgical repair. You may need a referral to a visiting nurse agency to help you heal your wound. All ways of treating pressure sores take a long time to work and require keeping pressure off the area. If you develop a pressure sore, talk with your nurse or doctor about it. Please see the chapter Pressure Sores for further information.
SKIN CARE
Nutrition for the Skin
Vitamins A, C, E, and B6 or niacin (NIGH-ah-sinn) are some key vitamins that are necessary for proper development and maintenance of healthy skin. These vitamins cannot function alone. They require adequate protein, calories, and other vitamins and minerals to carry out their function. These nutrients can be obtained by eating a well-balanced diet and a variety of foods. Some tips on how to eat a well-balanced diet can be found in the chapter on Nutrition.
Weight Control
Weight control is another area of concern for skin care. Being at an appropriate weight for your height may help lower your risk for skin breakdowns. To get an idea of what an appropriate weight for your height is or if you are underweight or overweight, see the chapter on Nutrition for tips on how to achieve your ideal weight.
Basic Hygiene
We all need regular hygiene (HIGH-jean). Dirt and grime, which normally contain different kinds of germs, settle on the surface of your skin. The total area of skin surface is approximately one square yard, which is a lot of breeding ground for tiny germs. Any cuts or scrapes of the skin will give these germs easy entry inside your body. Therefore, regular cleansing with soap and water by taking showers, tub baths, bed baths, or sponge baths is needed.
Daily bathing is encouraged during your younger and middle years. However, as you age, your skin becomes drier so daily whole body cleaning is not recommended. Skin should still be washed any time it is soiled. Areas such as armpits and groin still need daily cleaning.
Hygiene Tips Specific to SCI
Sitting in a wheelchair all day long with frequent weight shifts doesn't give air much of a chance to freely circulate in the groin area. Also, having your legs close together most of the day gives those normal body germs what they like most--a nice warm, dark, moist place to reproduce. And, if you're wearing some sort of plastic or rubber urine collecting device, such as condom catheter, foley catheter, waterproof padding, or leg bag, the chance of making that breeding ground more enticing to germs increases.
Hygiene Tips
- Wash your groin area again before going to bed for the night.
- Air out your groin area at least once a day by getting into the frog position.
- Always thoroughly dry your groin area and in between your toes after bathing.
- If you use powder, lightly dust some on your groin area. Be careful not to put on a lot. Too much powder can cake and cause lumps that could lead to irritation, rashes, and splits in your skin. Or you may also try using a stick antiperspirant along your groin creases to control the moisture.
- Clean your urine collecting equipment every day. See the chapter on Bladder Management for more information.
- Apply lotion daily to dry skin areas, except between your toes unless your doctor instructs you to do so. Dry skin can crack open.
- When doing nail care:
- Clean finger and toe nails daily.
- Keep your nails short for safety.
- Cut your toe mails straight across to prevent ingrown nails.
- Cut your nails after soaking them for 15-20 minutes or after taking a bath. This makes them easier to cut.
- Thick nails may need to be cut by a podiatrist or clinic nurse.
DAILY SKIN CARE SPECIFIC TO SCI
You need to give your skin special attention every day because of the decrease in circulation, lack of feeling, and lack of movement in your body below the level of your injury. Pressure sores can develop quickly. The need to recognize, treat, and, most of all, prevent them is very important. Examining your skin for possible problems is essential.
Tips for Skin Inspection
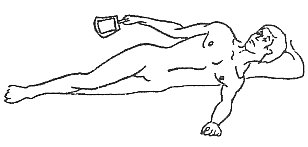
- Check your skin twice a day. Before you get out of bed, inspect those areas that have had pressure when you were lying down. After you get into bed, inspect those areas that have had pressure when you were sitting. (See figure 2.4.)
|
FIGURE 2.4. Skin Inspection Points
|
- Check all your bony places (ankles, elbows, heels, hips, tailbone) below the level of your injury. Use a mirror to see those bony areas behind you, like your sitting bones.
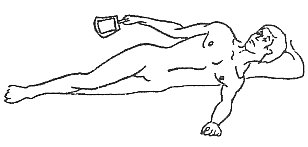
- If you cannot use a mirror or check your skin yourself, get someone (like your attendant) to check those areas for you.
- Look for reddened areas, cuts, scrapes, blisters, and bruises. Anything that seems different needs to be carefully checked out.
- If you find a reddened area, check the Troubleshooting section of this chapter for what to do next.
- Feel over the bony areas for changes like lumps or spots that are firmer than the rest of the skin around it.
Areas to Check
It is important to check the fit of your clothes, shoes, and equipment to be certain they are not too tight. Especially check the following items:
- Thick seams, especially on blue jeans.
- Binding in the groin area with pressure on your scrotum.
- Tight shoes, especially if you have swollen feet.
- Socks with elastic tops that bind around your lower leg.
- Straps holding your urine drainage system that are too tight.
- Condoms that have been applied too tightly.
Avoid These Problems
- Wash clothing that you have never worn before wearing and check your skin after one or two hours for redness or chafing.
- Buy jeans that are designed with low-profile seams (not bulky). Consider removing back pockets or buying jeans without them.
- Buy jeans and slacks in a size larger than your usual size to prevent constriction.
- If you are male, adjust your scrotum after you get dressed and transfer to your chair. Be certain that you are not sitting directly on your scrotum.
- Unless compression socks have been prescribed, wear socks that are neither too tight nor too loose.
- Check the fit of shoes carefully and watch your feet for signs of edema (swelling). After you have worn your shoes for 6 months or more, re-check the interior cushioning for signs of the padding wearing down.
- Loosen or change the position of your urine drainage system.
POSITIONING/TURNING
Changing your body posture takes pressure off your bony prominences. Listed below are some helpful tips for positioning/turning.
In Bed
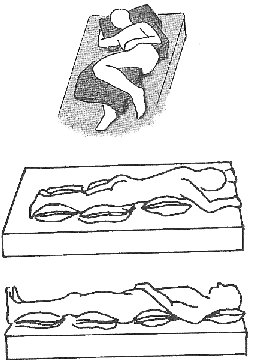
- Change your position according to your skin tolerance level. Use the routine of side to side to back for turns. Sleep on your stomach (prone), if possible. Note positioning of body parts and the use of pillows in the diagrams shown. (See figure 2.5.)
- When lying on your back in bed, avoid pressure on your heels by "suspending" your feet over the edge of a pillow. Some people wear special foot splints to protect the skin over the ankles or heels.
- Side-lying pressure on the fleshy part of your buttock will protect the skin over your hip bone (trochanter).
- Sitting in bed for prolonged periods is hazardous to the skin over your tail bone (sacrum, coccyx). So raise the head of the bed for short functional activities only.
|
|
FIGURE 2.5.
Positioning/Turning in Bed
|
|
- Use an alarm clock at first to wake you for your turns. After a while, turning in bed may become automatic for you.
- Get someone else to turn you (like your attendant) if you cannot do it for yourself.
- You may need a specialized mattress. Please discuss with your doctor or nurse.
|
In a Wheelchair
- Do pressure releases every 15 minutes to take the pressure off your tailbone and sitting bones. Ask your physical therapist for a set of diagrams of pressure-release methods.
Your options are listed below. Work with your therapist to find which is best for you.
- Push up out of the seat of your wheelchair with your hands slightly forward and hold for 30-60 seconds.
- Lean side to side staying in a side-leaning position for 30-60 seconds per tilt.
- Bend your chest forward onto your knees and hold this position for 30-60 seconds.
- Tilt your wheelchair back or use your recliner if you have one. Remain reclined for 1-2
minutes. Some people have developed skin problems when they remained in a reclined position for long periods of time (greater than 30 minutes).
- Shift your position as much as possible. Be a wiggle worm. It doesn't come automatically, but constant moving allows the blood to continue flowing.
- Check your posture by looking at yourself in a full length mirror after you are up in your wheelchair. Make sure that your ankles, the sides of your knees, and your hip bones are not leaning up against parts of your wheelchair. Your body has a natural balance and symmetry to it. Your knees and feet should appear to be "even". Spasticity and muscle strength imbalances can disrupt this balance and cause a change in your posture. Tight muscles in your trunk and legs can do the same. Things to look out for include:
- A curving or twisting of your back (spine).
- Tightness of your legs or your trunk that prevents your body from keeping its normal balance.
- One knee looking like it is "higher" than the other.
- Any appearance of "slumping" or leaning to one side of the wheelchair or the other.
- Make sure your foot pedals are adjusted for your height.
- Sit up as straight as possible in your wheelchair.
- Always use a WELL-MAINTAINED cushion.
- Be aware that any change in your positioning to ease pressure from one area will affect the pressure put on other areas.
PREVENTING INJURY
Before your spinal cord injury, your sensation warned you to move away from harm. Of course, accidents were always a possibility and will continue to be so.
After your spinal cord injury, you have lost some or all of the ability to feel and/or move below your level of injury. This puts you at risk for injury to your skin.
Tips in Preventing Injury:
- Always be aware of how close your paralyzed body parts are to possible hazards around you. Example: Are they too close to a heater, fireplace, campfire, or exposed hot water pipes? After transferring to an overstuffed chair, are your feet squarely on the floor?
- When transferring or moving around, be careful not to bump into things. Use your eyes to check out distances and obstacles. Remember that when you turn around in your wheelchair, your feet stick out farther than the rest of you, so wear shoes to protect your toes.
- Don’t do fancy or new maneuvers in your wheelchair until you have been trained.
- Spasms can lead to skin trauma. For example, a spasm during a tilt back can result in your ankle hitting a calf rest pad and causing injury.
- Do not sleep in your wheelchair, because you cannot do a pressure release if you are asleep.
POTENTIAL HAZARDS TO SKIN
Alcohol Abuse
Many people drink alcohol. Alcohol and other drug use may impair your judgment, which may lead to accidents or other activities that can injure you and your skin. When people are intoxicated, they forget to do pressure releases, so they are at risk for pressure sores.
Solutions
- To maintain clear thinking and good judgment, limit your alcohol intake. For example, drink alcohol only during meals and limit yourself to one or two drinks a day (1 drink = 12 oz. of beer, 6 oz. of wine, 1 oz. hard liquor). Please see the chapter on Nutrition.
- Do not drive a vehicle after drinking alcohol. Do not ride as a passenger in a vehicle driven by someone else who has been drinking alcohol.
- If alcohol or drug use is difficult to control, consult your health-care provider, a local mental health center, or a community alcohol treatment program.
Anemia
Anemia (ah-NEEM-ee-ah) is the medical term to describe a decreased number of red blood cells (RBCs). Almost all (97%) of the oxygen that gets to your tissues is carried there by your RBCs. If your RBCs are low, you are anemic (ah-NEEM-ick). If you do not have enough RBCs to carry oxygen to your cells, your skin is more prone to break down and, if it does break down, will be difficult to heal.
Solutions
There are many causes of anemia. One common cause of anemia is the lack of iron in your diet. You might try eating more red meats and green leafy vegetables or taking a vitamin with an iron supplement. You may benefit from consulting with a dietitian.
Cold Injuries
Your SCI puts you at risk for injury from things that are too cold because of the loss of skin sensation.
Solutions
- Beware of frozen foods on your lap. Use a pad underneath frozen items.
- If using ice over an area for swelling, wrap the ice in a towel. Do not ice longer than 10 minutes.
- Prevent frostbite by wearing warm socks and sturdy shoes when outside. Cover your head, ears, and hands when you go out. If your ears are becoming numb and tingling, your feet probably are too, so come inside!
Hot Injuries
Your SCI puts you at risk for injury from things that are too hot because of the loss of skin sensation.
Solutions
- Check the water temperature by putting a hand or other body part with feeling into the water and holding it there for five seconds. If you feel comfortable, the water temperature is safe. If you don’t have good sensation in your hand, have someone else check the water temperature or use a thermometer. Water temperature should typically range between 100° and 104°F for bathing.
- Be sure your hot water heater is not set higher than 120°F. Scalding burns occur very rapidly at temperatures greater than 120°F.
- Do not use a heating pad.
- Beware of feet being too near the heater of a car.
- Do not use electric blankets.
- Do not move too close to fireplaces, radiators, hot water pipes (especially under sink), or campfires.
- Do not carry hot fluids or foods in your lap without a tray. If you carry hot foods, use a sturdy board that covers the entire surface of the dish or pan to prevent burns from the hot container touching your leg.
- Use cup holders on your wheelchair.
- Do not fill cups too full.
- Keep pan handles over the stove surfaces to prevent bumping them.
- Do not wear loose-fitting long-sleeved shirts or reach across hot stove burners.
If you should burn yourself, initiate first aid treatment immediately. Apply cool water. Do not use ice or other frozen things on a burn.
If you spill hot food or fluids on yourself, you may not be able to detect all the places it came in contact with as it spilled. Pay close attention to your groin and buttocks areas.
Depression
For our definition, depression is not the feeling we all get from time to time of being down, gloomy, teary, or just fed up. A depressed person is someone who does not eat much, has no appetite, cannot sleep at night, or sleeps all the time. Depressed people also generally are very inactive and may neglect their self-care.
Depression itself does not cause problems to the skin, but the side effects of poor eating, sleeping, and not being active increases the likelihood of developing pressure sores from lack of movement.
Solutions
If you are just having a down day or two, don’t worry. It is normal and will probably pass. If it continues for longer than that, call your health-care provider and ask to talk to the psychologist or your nurse or doctor. Get help if your mood does not improve.
Stress
It is common for many people to become tense, nervous, or worried by the demands of their daily activities. Muscle tension, increased blood pressure, irritability, and fatigue are common symptoms of stress.
With constantly raised blood pressure and muscle tension, your body uses more energy, tires easily, and uses up the vitamins, minerals, and nutrients needed for healthy skin.
Solutions
- Read the chapter on Psychosocial Adjustment. It has a section that describes relaxation, time management, and stress reduction.
- Try to reduce your general stress level by taking time to relax every day.
Diabetes
Insulin is needed to get sugar into the cells for cell nutrition. When insulin is insufficient, sugar cannot get into the cells, and it builds up in the blood. That is why glucose (GLUE-kose), or blood sugar, is elevated in people who have diabetes.
Diabetes damages blood vessels and nerves. It can cause decreases in sensation in the hands and feet, which can lead to wounds. When a person has diabetes, wounds are more likely to become infected, and they heal much slower.
Solutions
- Control your blood sugar through diet, exercise, and use of medication if prescribed. Check your blood sugars as often as your health-care provider recommends.
- Inspect your skin closely for reddened areas, blisters, or sores. Pay particular attention to your feet and legs.
- Diabetic feet and toes are especially vulnerable to sores. Keep them clean and dry and your toenails trimmed. A tiny cut can lead to serious problems, so be careful to prevent injury.
- If you get a reddened area or sore, cover it to protect it from further injury. If the sore does not heal in one week after following the troubleshooting suggestions at the end of this chapter, call your health-care provider.
Edema
Edema (eh-DEEM-ah) is a condition in which fluid collects in and around tissues. It is seen as swelling, usually of the feet and ankles and sometimes in the hands if you are a quadriplegic.
If tissues swell too much, it is hard to get adequate oxygen and nutrients to the cells. That increases the likelihood of skin breakdown. If you do get a sore, it takes longer to heal because of the decreased supply of oxygen and nutrients.
Solutions
- Elevate your hands, legs, and feet frequently if these parts are affected.
- Wear your compression stockings or gloves if they are prescribed.
- Buy shoes one size larger to allow for swelling. Be aware of the amount of room from top to bottom in your shoe, not just the additional length, if you are prone to edema.
- Make sure your braces, splints, clothing, and urinary devices are not too tight, causing constriction.
If the edema continues and you want to know more, see the edema section in the chapter on Circulation.
Fever
When people get sick, they often run a fever. Fever is an elevated temperature. Usually a "normal" temperature is considered to be 98.6° Fahrenheit (F) or 37° Centigrade (C). However, it is common for some people to have their normal temperature slightly above or below 98.6° F. Temperatures also normally run higher in the afternoon and early evening than in the morning. There is no absolute normal. Learn what yours is. A fever is generally considered an elevation in temperature greater than 1.5 to 2° F or more than 0.8° C.
Your SCI may have affected your body's ability to regulate your temperature. Your body may now be very sensitive to the air temperature. After sitting in the hot sun for several hours, your body temperature may go up even though you are not sick. You may actually have a fever if your temperature rises to over 100° F.
An increased temperature is likely to make you sweat more. The additional moisture can cause your skin to be more likely to break down. It also increases your tissue's need for oxygen and nutrients, because your body is working harder to make you well again.
Solutions
- Carry a spray bottle of water to mist yourself if you will be out in hot weather for extended times.
- Wear a broad-brimmed hat.
- Drink more than your usual liquids to make up for the loss of fluid from fever or heat.
If you have a fever and you think you are sick, call your health-care provider. If you have a fever after you have been in the heat, take two acetaminophen tablets (650 mg total) every four hours. Take a cool bath or sponge yourself with a cool cloth, especially your head, neck, feet, hands, under your arms, and around your groin. If a fever lasts for more than one day, call your health-care provider.
Low Oxygen Levels
You can have a low oxygen problem if you have a lung, heart, or circulation disease. If you are a quadriplegic, your chest muscles are paralyzed and prevent you from taking deep breaths.
Tissues must have oxygen to live. When there is too little oxygen going to your skin, it is more likely to break down.
Solutions
If you have a low-oxygen problem, it is very important for you to read the chapter on Respiratory Care.
IF YOU SMOKE, STOP!
Follow your health-care providers’ recommendations.
Moisture
Anything that causes your skin to be wet or moist, including sweating, urine incontinence, or diarrhea, puts your skin at higher risk for breakdown.
Solutions
- Keep your skin clean and dry.
- Pay special attention to cleanliness in areas where you sweat.
- If you have skin folds, clean and dry under them well.
- Certain ointments or preparations with lanolin, petroleum jelly, or zinc oxide serve as barriers against moisture. If you develop a reddened area due to moisture, you might try one of these. Like other reddened area, pay close attention to it. If it does not go away in a week, call your health-care provider.
Underweight
Underweight means being 10% under your ideal body weight. See the Nutrition chapter to find your ideal body weight.
Some people who are underweight lack proteins, vitamins, and minerals. Low protein or vitamins can prolong the time it takes to heal a sore if you do develop one. If you are underweight, you may have less soft tissue padding between your sitting bones and skin for protection.
Solutions
Take in extra calories. If you get full quickly, eat more often. Make sure you get plenty of protein-rich food in your diet. If you have limited appetite, eat the nutritious foods first and save the junk food for later. You may also want to take a vitamin supplement. For more information, see the Nutrition chapter.
Overweight
Overweight is a relative term. Although there is a large range of weight that is acceptable, we will say that overweight is 10% or more over your ideal body weight. See the Nutrition chapter to find your ideal weight.
There are fewer blood vessels in fat tissue. Being overweight causes more pressure on your skin when you sit. This increased weight over pressure points increases the likelihood of skin breakdown.
Being overweight makes it harder for you to move your body around. Transfers are more difficult. Pressure releases may not be as effective.
Solutions
- Go on a weight-control program. To do so, see or call your dietitian. Read the chapter on Nutrition in this handbook.
- Keep areas between skin folds clean and dry. Inspect your skin twice a day for red areas.
- Change positions in bed every few hours. Do pressure releases every 15 minutes while sitting. You may need to do a different style of pressure release if you cannot lift your body.
- Maintain your activity level. Range of motion and being up in your wheelchair are activities. Your physical therapy or recreation therapist will have ideas for including aerobic exercise into your routine.
Peripheral Vascular Disease (PVD)
This is a term that means atherosclerosis (ATH-ear-o-sclurr-O-siss), or hardening of the arteries of the arms or legs (almost always the legs). This affects your circulation. It can be caused by diabetes, smoking, high blood pressure, and elevated cholesterol (kol-EST-er-all).
If the blood vessels are narrow, it is hard to get enough blood to the tissues. This increases the chance of the skin's breaking down by decreasing its oxygen and nutrient supplies.
Solutions
IF YOU SMOKE, STOP!
- If you have diabetes, try to keep your blood sugar in control.
- Keep your feet and legs warm. If your feet and legs are warm, the blood vessels will be as open as possible. If they are cold, the blood vessels will get smaller, which will make the problem worse.
- Keep your feet and legs very clean. Inspect them daily for sores or reddened areas. If you do get a sore that does not heal within a week, call your health-care provider.
Scar Tissue
A scar is any area of your skin where there was a break or cut in it and a mark, or scar, has formed. Scar tissue has fewer blood vessels and is less elastic than normal skin. It cannot withstand the same amount of pressure and will be more likely to break down.
Solutions
- Do careful skin inspections over areas with scars.
- Not all scars will turn red as the first sign of a problem; they may get white and feel hard to the touch. If the scar area starts getting reddened or becomes whiter for a long period, try to stay off it.
Smoking
The nicotine in cigarettes causes the blood vessels to constrict (get small). Smaller blood vessels decrease the amount of blood, oxygen, and nutrients that get to the tissues of the body. This includes the skin. The lack of oxygen and nutrients increases the likelihood of skin breakdown. In addition, hot ashes can fall on your skin and burn you.
Solutions
- The only way to prevent the effects of nicotine is to stop smoking. Stop-smoking classes are available. Contact your health-care provider.
- Use cigarette holders if you have impaired use of your hands.
- Knock the ashes off into an ashtray frequently.
- Hold the cigarette away from your body.
- Do not smoke in bed.
- Wear a fire-retardant cloth on your lap to keep ashes from burning you and your clothes.
- Install and maintain a smoke alarm in your home.
Sun
Your spinal cord injury has not changed your sensitivity to sunburn.
Solutions
- Use an SPF #15 or #25 sunscreen.
- To avoid burns, check sun-heated plastic, vinyl, or metal surfaces before you put any part of your body on them.
TROUBLESHOOTING FOR YOUR SKIN
Table 2.B. provides you with a comprehensive look at skin problems that may occur. This table includes a description of what you might see and what you can do to try to solve the problem.
TABLE 2.B. Troubleshooting for Your Skin
Let your spasticity be a clue to your health. If it gets worse, look for a problem. An example is spasticity that gets worse when you have a urinary tract infection. Any of the following skin problems can cause increased spasticity of your arms or legs.
| PROBLEM |
WHAT YOU SEE |
WHAT YOU DO |
| Blister |
Watery or bloody liquid (fluid) that can be seen under the skin. |
Do not pop. Keep pressure off it. If caused by heat, apply cold water soaks immediately. Cover with dry bandage. Phone health-care provider. |
| Boils |
A reddened, tender swelling containing clear fluid. |
Do not pop. Wash with mild soap twice a day. Phone health-care provider. |
| Bruise |
A blotchy, bluish-green discoloration of the skin. |
Cold compress initially. Keep pressure off bruise until cleared. |
| Burn |
Reddened or blistered skin caused by heat. May be an open sore. |
Apply cold water soaks immediately, then keep dry. Do not pop blisters. Do not use ice. Cover with dry bandage. Phone health-care provider. |
| Frostbite |
Whitened or bluish-black numb skin (usually nose, ears, fingers, toes) as a result of exposure to cold. |
Gradually and gently rewarm. Cool, then lukewarm water may be used to rewarm frozen parts. Do NOT use hot water bottles or other heat sources. Do NOT rub or massage. Phone health-care provider. |
| Groin Rash |
Reddened area in groin and found in creases and/or all over groin and penis. May be moist and/or pimply. |
Wash with mild soap and water 2-3 times a day. Rinse and dry well. Spread legs to air dry. If not better in 2-3 days, phone health-care provided. |
| Ingrown Toenail |
Reddened area around toenail, may have pus when pressed. Nail may be cutting into skin. |
Soak in soapy water, wash foot well, rinse, and dry. Put small piece of cotton under nail to keep edge of nail away from skin. Change cotton daily. Cut toenail straight across. If it does not begin to heal in 2-3 days, phone health-care provider. |
| Open Cut and Sores |
A wound in or through the skin. |
Apply pressure if bleeding. Wash with water or saline, rinse, and dry. Apply bandage. Keep pressure off of sore. Phone health-care provider if in area you have no feeling or if redness or pus is present. |
| Pimples |
Small reddened sores with a pus head on the skin. |
Do NOT pop. Wash twice a day with mild soap. Dry skin well. If pimples do not dry up, phone health-care provider. |
| Pressure Sores |
A sore usually over a bony area. See Pressure Sores Chapter. |
Wash with water or saline, rinse, and dry. Apply bandage if sore is open. Keep all pressure off the sore. Phone health-care provider. |
| Red Area |
Red skin that does not fade in 15 minutes. Does not blanch (turn white when pressure is put on it). |
Do not put pressure on the area until the redness fades completely. May take days. |
| Sunburn |
Dry, red skin with or without blisters, fever. |
Apply cold water soaks to skin for comfort, then soothing creams. Do NOT pop blisters. Cover blisters with bandage. If fever persists, call health-care provider. |
| Swelling |
An abnormal enlargement or increase in size of body part, usually on arms or legs. May also have color change-red or black and blue. |
Elevate the swollen part and wear your compressive hose. See the chapters on Nerve, Muscles & Bones and Circulation. If swelling is not even from one side to the other, call your health-care provided. |
|
RESOURCES
Publications
Preventing Pressure Ulcers: A Patient’s Guide
Treating Pressure Sores: A Consumer’s Guide
Purchase:
AHCPR Publications Clearinghouse
P.O. Box 8547
Silver Spring, MD 20907-8547
(800) 358-9295
Download: www.ahcpr.gov
Web Sites
www.healthpages.org/AHP/LIBRARY/HLTHTOP/MISC/bedsore.htm
A web site dedicated to preventing pressure ulcers.
www.woundcarenet.com/educat/press3.htm
The on-line skin and wound care resource from the publisher of Advances in Skin & Wound Care and the joint sponsor of the annual Clinical Symposium on Advances in Skin & Wound Care.
Organizations
Wound, Ostomy and Continence Nurses Society (WOCN)
An association of ET nurses, WOCN is a professional nursing society that supports its members by promoting educational, clinical, and research opportunities to advance the practice and guide the delivery of expert health care.
The National Decubitus Foundation
The goals of the organization are to increase public awareness in the areas of education, research, and advocacy for the proper care of individuals with decubitus ulcers.
|